The CMS Rule and What It Changes for Home Care Agencies
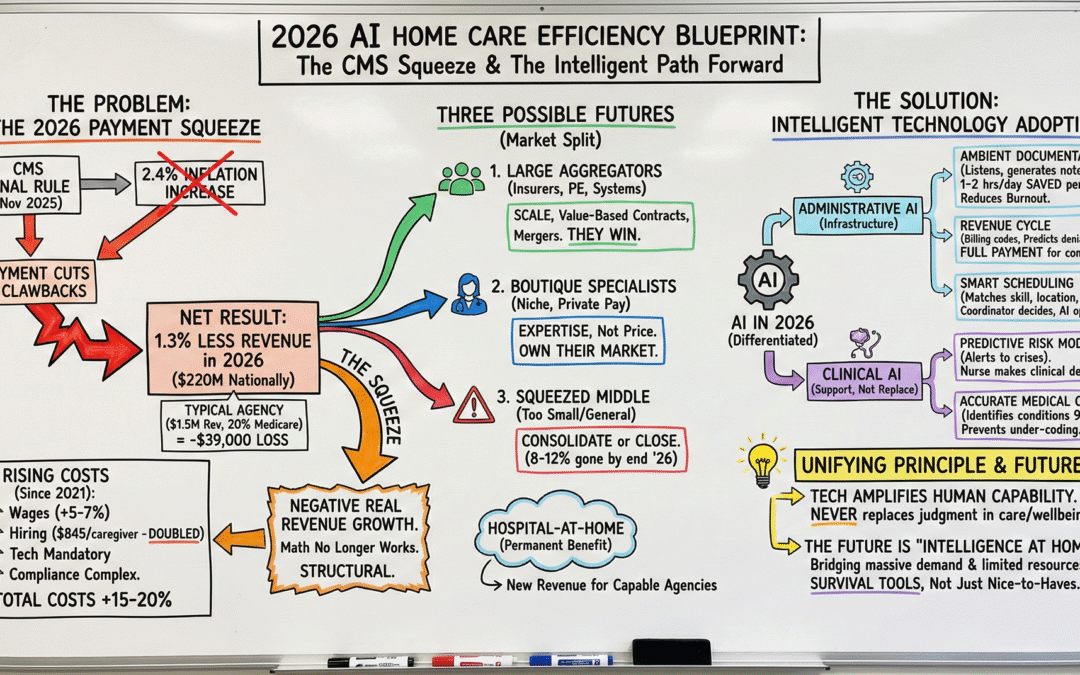
On November 28, 2025, the government finalized its payment rules for home care agencies in 2026. The headline: a 2.4% increase to cover inflation.
The reality: that increase gets completely erased by payment cuts. Agencies will actually receive 1.3% less in 2026 than in 2025. That’s a $220 million reduction nationally.
For a typical agency with $1.5 million in revenue where 20% comes from Medicare, that’s a $39,000 loss. Meanwhile, worker wages are climbing 5-7% due to inflation. Hiring costs $845 per new caregiver (up from $400 five years ago).
The math no longer works.
This isn’t temporary. This is structural. Agencies cannot solve this through cost-cutting or payment advocacy. There is only one path forward: intelligent technology adoption combined with unwavering commitment to worker wellbeing.
Why This Is Happening
To understand 2026, you need to know what changed over the last five years.
Costs increased 15-20% from 2021 to 2026
Wages rose. Hiring costs doubled. Technology became mandatory infrastructure. Compliance grew more complex.
Revenue decreased
Medicare cut payments in 2023 (3.9%), 2024 (2.9%), and 2026 (1%), plus implemented a 3.0% clawback to recoup what it considers “historical overpayments.” When adjusted for inflation, agencies are earning less than they did five years ago. This is Negative Real Revenue Growth.
Technology adoption exploded
In 2021-2022, 20% of agencies used modern software. Today, 80% operate on cloud-based electronic health record systems. AI tools for documentation, scheduling, billing, and hiring are emerging rapidly. Agencies that have deployed these tools report 56% operational efficiency improvements.
What was optional in 2021 is mandatory in 2026.
What This Means: Three Possible Futures
The payment squeeze is creating a market split.
Large aggregators (insurance companies, health systems, private equity) have capital to invest in intelligent technology. They absorb margin pressure through scale. They negotiate value-based contracts with hospitals: “We reduce your readmissions, you pay us better.” Merger activity is at its highest level in two years. These companies win.
Boutique specialists focus on one niche: pediatric, hospice, or complex wound care. Or they serve wealthy private-pay clients. They don’t compete on price; they compete on expertise. They own their market.
The squeezed middle: agencies too small to scale, too general to specialize. These face consolidation or closure. By end of 2026, expect 8-12% of independent Medicare-certified agencies to be gone.
Additionally, Hospital-at-Home programs are becoming permanent. Major health systems have made serious capital investments. By late 2026, what was temporary becomes a permanent Medicare benefit. Agencies capable of managing complex patients will have a new revenue stream. Agencies that can’t will see hospitals build their own programs or contract with large aggregators instead.
What Intelligent Technology Actually Does
AI in 2026 isn’t one thing. It’s differentiated into two categories.
Administrative AI: The Essential Infrastructure
Ambient documentation: AI listens to nurse-patient conversations and automatically generates required clinical notes. Real result: 15,791 hours saved annually per agency. That’s 1-2 hours daily per nurse freed from documentation burden.
This matters because it honors the humans doing the work. Nurses reclaim time for actual patient connection. Burnout decreases. Retention improves.
Revenue cycle management: AI figures out billing codes, checks insurance coverage, and predicts denials 95% of the time before submission. This ensures agencies claim full payment for the complexity they serve.
Smart scheduling: Algorithms match nurses to patients based on location, skills, personality fit, and retention risk. The coordinator still makes the final decision. The algorithm is a tool, not a replacement.
Clinical AI: Support, Not Replacement
Predictive risk modeling: AI analyzes patient data and alerts clinicians to potential medical crises before they occur. But qualified nurses make all clinical decisions. AI provides possibilities; humans provide wisdom.
Accurate medical coding: AI identifies 97% of patient conditions from clinical notes with 95% accuracy. This prevents under-coding that leaves thousands on the table.
The Unifying Principle
Every ethical AI application follows one rule: Technology amplifies human capability. It never replaces human judgment in matters touching patient care or worker wellbeing.
The coordinator remains the decision-maker. The nurse remains the clinical authority. The agency maintains accountability. Technology handles pattern-matching and optimization. It’s the work that’s been stealing hours from human attention.
Where This Goes
Home care in 2026 is caught between two forces: massive demographic need and shrinking government resources.
The agencies that will thrive are those that understand what intelligent technology can do. Not as a cost-cutting measure, but as a way to reclaim time, improve accuracy, and support the people doing the work.
Agencies deploying ambient documentation are freeing nurses from 1-2 hours of daily documentation burden. Agencies with smart scheduling are matching nurses to patients more effectively. Agencies with accurate AI billing are claiming full payment for the complexity they serve.
These aren’t nice-to-haves. When revenue is declining and costs are rising, they’re survival tools.
The future of home care is “intelligence at home”. Technology that bridges the gap between massive demand and limited resources.
Ready to explore your options?
If you’re an agency owner navigating the 2026 squeeze, let’s talk about what’s possible in your operation.
Schedule a Discovery Call | Try the ROI Calculator
Neurvana AI partners with independent home care agencies to eliminate scheduling chaos and protect margins. We work alongside your team to transition from labor-intensive operations to intelligent care platforms.
Contact: Luke McNeur, Founder | lukemc@neurvana.ai